Understanding Screen 5 of the Plan Setup
The requirements of third party plans can vary from payer to payer. HIPAA states that only the information requested by the payer via their published payer sheet be transmitted in a claim transaction.
To address that requirement, we’ve given you a great deal of flexibility when defining what information is transmitted to the end payer. Screen 5 of the plan setup defines what information is sent, and what type of transaction the information is sent in. Below you will see a screen shot of page 5 along with an overview of the information displayed.
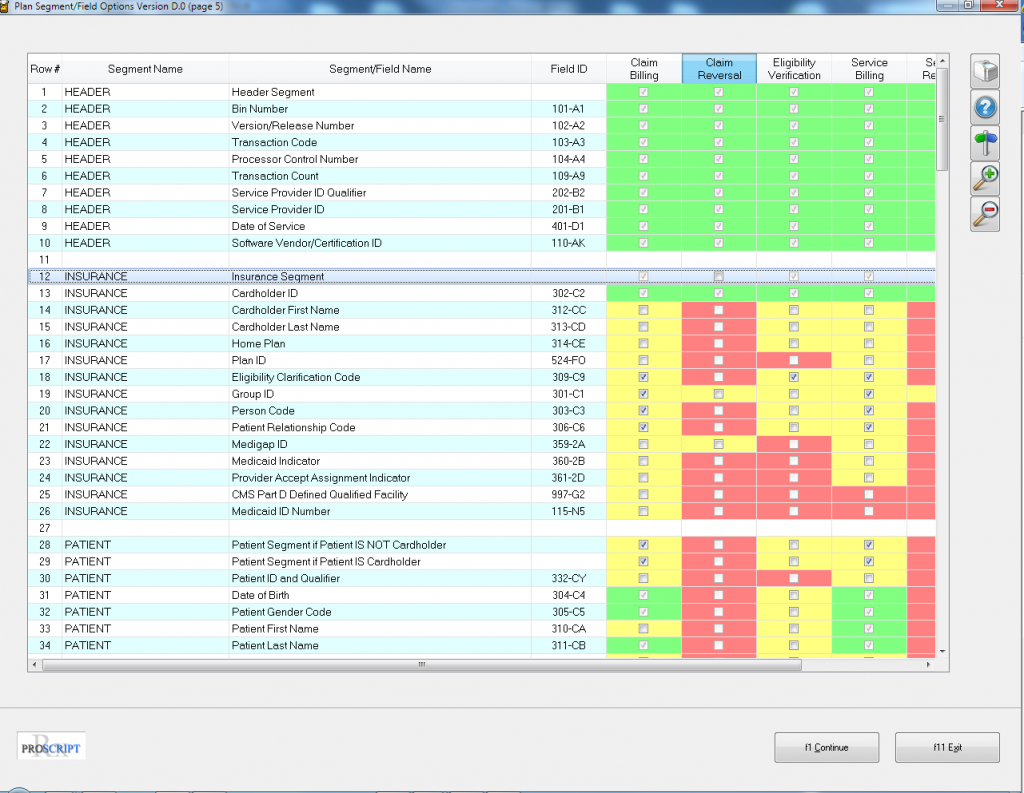
Segment Name – Claim information is separated into segments when the claim is transmitted and received. Occasionally a payer will return the segment name when returning a rejected claim. This helps you determine what piece of information is missing in the claim.
Segment/Field Name – Within each segment, there are multiple fields. Payers will typically return this field on a rejected claim. This helps you determine what piece of information is missing in the claim.
Field ID – Each field has a unique Field ID number. Payers will almost always return this field on a rejected claim. This helps you determine what piece of information is missing in the claim.
Checkbox Columns – Each column represents a different transaction type; Claim Billing, Claim Reversal, Eligibility Verification, Service Billing and Service Reversal. The fields in the columns are color coded:
Green – This field will be transmitted for the transaction type represented by the column in question by default.
Yellow – This field is optional and will only be transmitted if there is a checkbox in the field of the transaction type represented by the column in question.
Red – This field is not available for the transaction type represented by the column in question.
So, you have control over what is sent. For example, let’s assume that you have sent a claim to a payer and have received a reject stating “Missing/Invalid Patient First Name”. You can come to the screen in the plan setup and place a check in the Claim Billing column for the field Patient First Name. This will now tell the system to send the patient’s first name when submitting the claim.